Sessions & Tracks
Track 1: Nephrology
Nephrology is the branch of the medical practice of adult internal medicine and pediatric medicine that deals with the study of kidneys, their treatment, and preservation of kidney health. It also studies the factors affecting kidneys (diabetes and high blood pressure), systemic diseases like hypertension, renal osteodystrophy. Many diseases that affect the kidneys often are not limited to the organ itself, they affect other organs in the body and can cause lupus, urinary tract infections (UTI), and polycystic kidney disease which require special treatment. Many treatments associated with kidney include kidney dialysis, fistula management, kidney, and bone biopsy. Tests and procedures to determine the diagnosis of kidney diseases are blood tests, urine tests, ultrasound imaging tests, and kidney biopsy to remove a sample of kidney tissue for testing.
Related associations and societies: International Society of Nephrology (ISN), American Society of Nephrology (ASN), UK Kidney Association (UKKA), Canadian Society of Nephrology (CSN), Hong Kong Society of Nephrology (HKSN), Saudi Society of Nephrology and Transplantation (SSN&T), Australian and New Zealand Society of Nephrology (ANZSN), Malaysian Society of Nephrology (MSN), National Kidney Foundation (NKF), California Dialysis Council (CDC), International Society for Hemodialysis (ISHD), American Society of Transplantation (AST)
Track 2: Impact of Covid-19 on Nephrology
People with kidney diseases and chronic medical conditions are at higher risk of viral infectious diseases. People who are undergoing dialysis have a lower immune system which makes it difficult for them to fight infections. Coronavirus side effects in an acute kidney injury include acute tubular necrosis with septic shock, direct infection to the kidney, and an increase in blood clotting. There are chances the function of kidneys declines after contracting with coronavirus and during infection. Nephrologists have observed high levels of protein in the urine (Proteinuria) in patients having COVID-19. Though researchers and medical professionals have not recommended patients stop using a particular drug, taking precautions is always a must. Getting vaccination shots, maintaining good hygiene, taking medicines as prescribed, consulting the doctor timely is important.
Related associations and societies: National Kidney Foundation (NKF), California Dialysis Council (CDC), International Society for Hemodialysis (ISHD), American Society of Transplantation (AST), International Society of Nephrology (ISN), American Society of Nephrology (ASN), UK Kidney Association (UKKA), Canadian Society of Nephrology (CSN), Hong Kong Society of Nephrology (HKSN), Saudi Society of Nephrology and Transplantation (SSN&T), Australian and New Zealand Society of Nephrology (ANZSN), Malaysian Society of Nephrology (MSN)
Track 3: Renal Pathology
Renal pathology deals with the characterization of medical diseases (non-tumors) and the diagnosis of kidneys. Renal pathologists work along with nephrologists and kidney transplant surgeons who specialized in the diagnosis of medical diseases of the kidneys. The pathologist interprets the biopsy tissue in the clinical context, synthesizes findings from microscopy, electron microscopy, and finds out the diagnosis. Medical renal diseases may affect the tubules and interstitium, the glomerulus, the vessels, or a combination of these departments.
Related associations and societies: International Society of Nephrology (ISN), American Society of Nephrology (ASN), UK Kidney Association (UKKA), Canadian Society of Nephrology (CSN), Hong Kong Society of Nephrology (HKSN), American Society of Transplantation (AST), Saudi Society of Nephrology and Transplantation (SSN&T), Australian and New Zealand Society of Nephrology (ANZSN), Malaysian Society of Nephrology (MSN), National Kidney Foundation (NKF), California Dialysis Council (CDC), International Society for Hemodialysis (ISHD)
Track 4: Renal Replacement Therapy
Renal replacement therapy replaces the blood filtering function that the kidneys perform normally. The therapy is recommended for patients who are suffering from kidney failure, acute kidney injury, and chronic kidney disease when the kidneys are not working well. Kidney transplantation is the ultimate form of replacing the old kidney with the donor's kidney. Renal replacement therapy also includes filtration of blood with or without the help of machines, hemofiltration, hemodiafiltration, and also dialysis. Therapy is often viewed to be a life-extending treatment and not a cure for kidney disease, although if the disease is managed well with dialysis and early diagnosis, the results are quite favorable. The available renal replacement therapies include peritoneal dialysis (PD), intermittent hemodialysis (IHD), and continuous renal replacement therapy (CRRT).
Related associations and societies: International Society of Nephrology (ISN), Australian and New Zealand Society of Nephrology (ANZSN), Malaysian Society of Nephrology (MSN), National Kidney Foundation (NKF), American Society of Nephrology (ASN), UK Kidney Association (UKKA), Canadian Society of Nephrology (CSN), Hong Kong Society of Nephrology (HKSN), Saudi Society of Nephrology and Transplantation (SSN&T), California Dialysis Council (CDC), International Society for Hemodialysis (ISHD), American Society of Transplantation (AST)
Track 5: Pediatric Nephrology
A study where a pediatric nephrologist treats kidney or urinary tract disease, bladder problems, and high blood pressure of children from infancy through late adolescence years is called pediatric nephrology. Pediatric nephrology includes treating dialysis, kidney biopsy, kidney transplantation, interpretation of the kidneys through x-ray studies, and blood pressure monitoring. Children getting affected by kidney diseases can be treatable disorders to life-threatening conditions. Certain birth defects, hereditary problems, infection, urine blockage or reflux, systemic diseases like lupus erythematosus and diabetes, and nephrotic syndrome are causes of kidney disease in children. Comprehensive disease management is key to keeping kidney diseases in check and preventing the growth of it, anemia, and other complications among children.
Related associations and societies: International Society of Nephrology (ISN), American Society of Nephrology (ASN), UK Kidney Association (UKKA), Australian and New Zealand Society of Nephrology (ANZSN), Malaysian Society of Nephrology (MSN), National Kidney Foundation (NKF), California Dialysis Council (CDC), International Society for Hemodialysis (ISHD), American Society of Transplantation (AST), Canadian Society of Nephrology (CSN), Hong Kong Society of Nephrology (HKSN), Saudi Society of Nephrology and Transplantation (SSN&T)
Track 6: Clinical Nephrology
Clinical nephrology is the fame of medicine that analyzes the working of kidneys, their functioning, and treatment is given as per the analysis from the form of kidney functioning, renal transplantation to the newest transplant techniques. It is a branch of therapeutics and pediatrics that is concerned about the investigation of kidney function, Nephrology maladies, the treatment of Nephrology ailments, and renal transplantation treatment (dialysis and kidney transplantation). Kidneys play a vital role in life with their complex network of blood vessels and intricate network of tubes and tubules that filter the blood of its waste products and excess water. Kidneys maintain liquids, electrolytes, and corrosive base direction that are modified by kidney malady conditions and in addition drugs and toxins. Kidneys perform several functions and clinical nephrologists tend to maintain expertise in primary kidney disorders.
Related associations and societies: American Society of Transplantation (AST), International Society of Nephrology (ISN), American Society of Nephrology (ASN), UK Kidney Association (UKKA), Canadian Society of Nephrology (CSN), Hong Kong Society of Nephrology (HKSN), Saudi Society of Nephrology and Transplantation (SSN&T), Australian and New Zealand Society of Nephrology (ANZSN), Malaysian Society of Nephrology (MSN), National Kidney Foundation (NKF), California Dialysis Council (CDC), International Society for Hemodialysis (ISHD)
Track 7: Chronic Kidney Disease
Chronic kidney disease (CKD) is a kidney disorder where the functioning of kidneys tends to stop after a while (months to years). The kidneys can’t filter blood the way kidneys should and it damage which causes wastes to build up in the body and may cause other health problems like heart disease and stroke. Though there are no initial symptoms in general, some of the common symptoms observed later are leg swelling, loss of appetite, feeling tired, vomiting, and confusion. Increased risk of heart disease, high blood pressure, hypertension, polycystic kidney disease, and glomerulonephritis are some of the causes of chronic kidney disease. Early screening and initial treatments include medications to lower blood pressure, sugar, and cholesterol levels.
Related associations and societies: National Kidney Foundation (NKF), International Society of Nephrology (ISN), American Society of Nephrology (ASN), UK Kidney Association (UKKA), Canadian Society of Nephrology (CSN), Hong Kong Society of Nephrology (HKSN), Saudi Society of Nephrology and Transplantation (SSN&T), Australian and New Zealand Society of Nephrology (ANZSN), Malaysian Society of Nephrology (MSN), California Dialysis Council (CDC), International Society for Hemodialysis (ISHD), American Society of Transplantation (AST)
Track 8: Acute Kidney Failure
The sudden dysfunction of kidneys where they cannot filter waste from the blood is called acute kidney failure. Kidney failure develops rapidly in a few hours or days and maybe fatal. Symptoms are swelling due to fluid retention, decreased urinary output, and shortness of breath, fatigue, and nausea. Acute kidney failure can occur when patients have experienced direct damage to the kidneys, when you have a condition that slows down blood flow to the kidneys and when kidneys urine drainage tubes (ureters) become blocked and the waste cannot leave your body through urine. Risk factors are often observed in connection with other medical conditions like liver diseases, heart failure, certain cancers, and their treatments, being hospitalized for a serious condition that required intensive care.
Related associations and societies: American Society of Transplantation (AST), International Society of Nephrology (ISN), American Society of Nephrology (ASN), UK Kidney Association (UKKA), Canadian Society of Nephrology (CSN), Hong Kong Society of Nephrology (HKSN), Saudi Society of Nephrology and Transplantation (SSN&T), Australian and New Zealand Society of Nephrology (ANZSN), Malaysian Society of Nephrology (MSN), National Kidney Foundation (NKF), California Dialysis Council (CDC), International Society for Hemodialysis (ISHD)
Track 9: Hematuria and Proteinuria
The presence of blood or red blood cells in urine is called hematuria. The causes of hematuria are infection occurred in the urinary tract, bladder, kidney or bladder cancer, inflammation of the kidneys, or prostate and polycystic kidney disease. There are two types of hematuria and they are microscopic and gross hematuria. The Non-visible hematuria (microscopic hematuria) means that the blood can only be seen with a microscope whereas visible hematuria (gross hematuria) means the urine appears red or the color of tea or cola to the naked eye. Urine tests, blood tests, CT scans, kidney ultrasounds, cystoscopy, kidney biopsy are the tests available to determine the hematuria and the cause of it, and not all tests are recommended to anyone.
Proteinuria is observed when an excess of protein is present in the urine which can be a sign of kidney damage. When the kidneys are damaged, the filters in the kidneys let proteins such as albumin leak from the blood into the urine. Dietary changes, weight management, blood pressure, and diabetes medication, and dialysis are the treatments nephrologists ask the patients to maintain.
Related associations and societies: Hong Kong Society of Nephrology (HKSN), International Society of Nephrology (ISN), Saudi Society of Nephrology and Transplantation (SSN&T), Australian and New Zealand Society of Nephrology (ANZSN), American Society of Nephrology (ASN), UK Kidney Association (UKKA), Canadian Society of Nephrology (CSN), Malaysian Society of Nephrology (MSN), National Kidney Foundation (NKF), California Dialysis Council (CDC), International Society for Hemodialysis (ISHD), American Society of Transplantation (AST)
Track 10: Urology
The branch of medicine that focuses on the medical diseases of the male and female urinary tract systems and male reproductive organs is called urology. Both the urinary and reproductive tracts are closely linked and if disorders of one often tend to affect the other. Urological techniques include invasive robotic and laparoscopic surgery, laser-assisted surgeries, and other scope-guided techniques. Urologists receive training in open and minimally interfering surgical techniques, employing real-time ultrasound guidance, fiber-optic endoscopic equipment, and various lasers in the treatment of multiple benign and harmful conditions. Urology is associated with urologists who often collaborate with different department practitioners related to oncology, nephrology, gynecology, andrology, pediatric surgery, colorectal surgery, gastroenterology, and endocrinology.
Related associations and societies: Saudi Society of Nephrology and Transplantation (SSN&T), Australian and New Zealand Society of Nephrology (ANZSN), Malaysian Society of Nephrology (MSN), National Kidney Foundation (NKF), International Society of Nephrology (ISN), American Society of Nephrology (ASN), UK Kidney Association (UKKA), Canadian Society of Nephrology (CSN), Hong Kong Society of Nephrology (HKSN), California Dialysis Council (CDC), International Society for Hemodialysis (ISHD), American Society of Transplantation (AST)
Track 11: Urinary Tract Infections
Urinary tract infections (UTIs) are infections that are related to any parts of the urinary system such as kidneys, bladder, or urethra. Often observed in women, urinary tract infections occur in the bladder or urethra, but serious infections involve the kidney. Female anatomy, sexual activity, certain types of birth controls, menopause, urinary tract abnormalities, blockages in the urinary tract, suppressed immune system, catheter use and recent urinary procedure are the risk factors specific to women who have urinary tract infections. They are often treatable and are short-term infections. Maintaining healthy hygiene, staying hydrated, the practice of good sexual hygiene, urinating when the need arises prevents UTIs. In men, prostate problems cause urinary tract infections and sexually transmitted diseases are the most common cause of UTIs in younger men.
Related associations and societies: International Society for Hemodialysis (ISHD), American Society of Transplantation (AST), International Society of Nephrology (ISN), American Society of Nephrology (ASN), UK Kidney Association (UKKA), Canadian Society of Nephrology (CSN), Hong Kong Society of Nephrology (HKSN), Saudi Society of Nephrology and Transplantation (SSN&T), Australian and New Zealand Society of Nephrology (ANZSN), Malaysian Society of Nephrology (MSN), National Kidney Foundation (NKF), California Dialysis Council (CDC)
Track 12: Hydro Nephrosis
The building up of excess fluid in a kidney due to back-up of urine is characterized as hydronephrosis. Hydronephrosis can occur in either one or both the kidneys and kidneys swell up as urine cannot be drained out from the kidney to the bladder from the blockage or obstruction. Kidney stones or infections are often caused by problems because of hydronephrosis and in men over the age of 50 (due to enlargement of the prostate), sexually active women are at higher risk of this condition. An ultrasound scan that uses sound waves to picture the inside of the kidney is done to diagnose hydronephrosis and further tests are conducted to know the exact condition. The treatments include antibiotics if there is an infection and in severe cases, urine needs to be drained from the kidney or bladder.
Related associations and societies: Canadian Society of Nephrology (CSN), Hong Kong Society of Nephrology (HKSN), Saudi Society of Nephrology and Transplantation (SSN&T), International Society of Nephrology (ISN), American Society of Nephrology (ASN), UK Kidney Association (UKKA), Australian and New Zealand Society of Nephrology (ANZSN), Malaysian Society of Nephrology (MSN), National Kidney Foundation (NKF), California Dialysis Council (CDC), International Society for Hemodialysis (ISHD), American Society of Transplantation (AST)
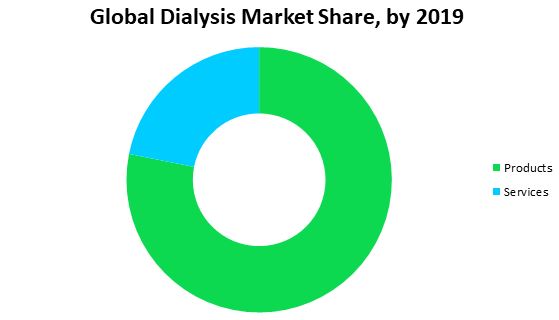
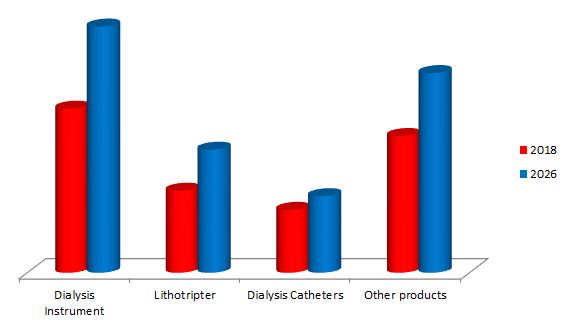
Track 13: Dialysis
The process of removing waste products, excess water, toxins, and solutes from the blood in people whose kidneys no longer function naturally is called dialysis. Dialysis involves diverting blood to be cleaned. Haemodialysis dialysis and peritoneal dialysis are two types of dialysis. Haemodialysis, the most common type of dialysis procedure where a tube is attached to a needle in your arm and the blood passes along the tube, and external machine filters the blood before it is passed back into the arm along another tube. The peritoneal dialysis process on the other side uses the inside lining of your abdomen (the peritoneum) as the filter, instead of a machine. The peritoneum contains thousands of tiny blood vessels, making it a useful filtering device just like the kidneys. Dialysis treatment can be stopped if the kidney disease is temporary and the patients get recovered.
Related associations and societies: International Society of Nephrology (ISN), American Society of Nephrology (ASN), UK Kidney Association (UKKA), Canadian Society of Nephrology (CSN), Hong Kong Society of Nephrology (HKSN), California Dialysis Council (CDC), International Society for Hemodialysis (ISHD), American Society of Transplantation (AST), Saudi Society of Nephrology and Transplantation (SSN&T), Australian and New Zealand Society of Nephrology (ANZSN), Malaysian Society of Nephrology (MSN), National Kidney Foundation (NKF)
Track 14: Diabetic Nephropathy
Diabetic nephropathy also called diabetic kidney disease caused by type 1 and type 2 diabetes is a complication that affects the kidneys. It affects the ability of kidneys of removing waste and fluid from the body. Diabetic nephropathy can slowly damage the kidney's filtering system but early treatment may prevent or slow down the disease progress. Dialysis and kidney transplantation are the treatment options if diabetic nephropathy leads to kidney failure which is end-stage kidney disease. Diabetes can increase the risk factors of diabetic nephropathy which include hyperglycemia, hypertension, and high blood cholesterol, and obesity, hereditary and smoking habits. Adequately managing diabetes and high blood pressure, maintaining a healthy lifestyle is the way to prevent or delay diabetic nephropathy.
Related associations and societies: International Society of Nephrology (ISN), American Society of Nephrology (ASN), Canadian Society of Nephrology (CSN), Hong Kong Society of Nephrology (HKSN), Saudi Society of Nephrology and Transplantation (SSN&T), Australian and New Zealand Society of Nephrology (ANZSN), Malaysian Society of Nephrology (MSN), National Kidney Foundation (NKF), California Dialysis Council (CDC), International Society for Hemodialysis (ISHD), American Society of Transplantation (AST), UK Kidney Association (UKKA)
Track 15: Renal Nutrition & Diet
Compromised kidney functions people are often advised to follow a renal diet that is low in sodium, phosphorous, and protein as to cut down the amount of waste in their blood. The kidneys do not tend to remove waste and fluids properly when they are compromised kidneys. The renal nutrition and diet emphasize maintaining a balance between food intake and usually limiting fluids. Every person’s body is different and so are their requirements so a renal dietician tailors a diet according to their need. Kidney patients monitor sodium intake as kidneys cannot eliminate excess sodium and fluid. Kidney failure can no longer remove excess potassium and thus it causes hyperkalemia and to avoid that, paying attention to serving size, choosing fresh produce, limiting dairy products, and substituting salt with other spices help. Monitoring phosphorus intake as high levels of phosphorus can pull calcium out of the bones, and make them weak so avoiding the word “PHOS” on ingredient labels, eating smaller portions, and choosing foods that have low phosphorous.
Related associations and societies: Australian and New Zealand Society of Nephrology (ANZSN), Malaysian Society of Nephrology (MSN), National Kidney Foundation (NKF), California Dialysis Council (CDC), International Society for Hemodialysis (ISHD), American Society of Transplantation (AST), International Society of Nephrology (ISN), American Society of Nephrology (ASN), UK Kidney Association (UKKA), Canadian Society of Nephrology (CSN), Hong Kong Society of Nephrology (HKSN), Saudi Society of Nephrology and Transplantation (SSN&T)
Track 16: Kidney Transplantation
Surgery performed to replace a diseased kidney with a healthy kidney from a donor is called a kidney transplant. A person might need a kidney transplant when they are at end-stage renal disease (ESRD) which is a permanent condition of kidney failure that requires dialysis. Often family members are a good match or others donate one of their kidneys. Donors can be living or deceased one and the living donors can lead a healthy life with one healthy kidney. The new kidney is placed in the lower abdomen. Complications after the kidney transplant include bleeding, infection, blockage of urine in the ureter, blockage of the blood vessels in the new kidney. Kidney transplant recipients are given immunosuppressants to prevent the body from rejecting the new kidney and long-term use of immunosuppressants puts the kidney transplant patients at higher risk for infections and cancer. Current issues associated with kidney transplantation are kidney allocation policies, xenotransplantation, transplant tourism, tolerance, and kidney transplantation clinical trials.
Related associations and societies: International Society of Nephrology (ISN), American Society of Transplantation (AST), American Society of Nephrology (ASN), UK Kidney Association (UKKA), Canadian Society of Nephrology (CSN), Hong Kong Society of Nephrology (HKSN), Saudi Society of Nephrology and Transplantation (SSN&T), Australian and New Zealand Society of Nephrology (ANZSN), Malaysian Society of Nephrology (MSN), National Kidney Foundation (NKF), California Dialysis Council (CDC), International Society for Hemodialysis (ISHD)
Track 17: Drugs and Medication for Kidney Disease
Drugs that are suggested for people with kidney diseases are always based on medical history and lifestyle. Nephrologists, the doctors who treat kidney diseases and health give brief about the side effects if any as well while prescribing drugs to the patients. Co-trimoxazole is an antibiotic that is advised to take after the kidney transplant or when you are taking cyclophosphamide (immunosuppressant) or rituximab. Isoniazid is a drug that may be prescribed after a kidney transplant for patients who may come into contact with or have previously had tuberculosis (TB) which is a long-term infection that affects the lungs, chest, or at times any part of the body. Azathioprine, ciclosporin, and mycophenolate medicines also come under immuno-suppressants that are recommended for kidney diseases. Cyclophosphamide, also an immune suppressant is taken in bigger doses to treat cancers. Cyclophosphamide medicine is prescribed to be taken for myeloma, vasculitis, lupus, or membranous nephritis. Along with this, following a balanced diet or a renal diet is often recommended to have a healthy lifestyle for kidney disease suffering patients.
Related associations and societies: Australian and New Zealand Society of Nephrology (ANZSN), Malaysian Society of Nephrology (MSN), National Kidney Foundation (NKF), California Dialysis Council (CDC), International Society for Hemodialysis (ISHD), American Society of Transplantation (AST), International Society of Nephrology (ISN), American Society of Nephrology (ASN), UK Kidney Association (UKKA), Canadian Society of Nephrology (CSN), Hong Kong Society of Nephrology (HKSN), International Society of Nephrology (ISN), American Society of Nephrology (ASN), UK Kidney Association (UKKA), Canadian Society of Nephrology (CSN), Hong Kong Society of Nephrology (HKSN)
Track 18: Renal Cell Cancer
Renal cell cancer is a kidney cancer disease in which malignant (cancer) cells are present in the lining of tubules (very small tubes) in the kidney. Tiny tubules which are present in the kidneys filter out waste and clean the blood. Smoking and misuse of certain pain medicines, overweight, high blood pressure; a family history of renal cell cancer can affect the risk of renal cell cancer. In the early stages, no signs and symptoms of renal cell cancer are observed but signs and symptoms may appear as the tumor grows. They are blood in the urine, a lump in the abdomen (belly), loss of appetite, pain in the side that doesn't go away, weight loss for no known reason, and fatigue.
Related associations and societies: National Kidney Foundation (NKF), California Dialysis Council (CDC), International Society for Hemodialysis (ISHD), American Society of Transplantation (AST), International Society of Nephrology (ISN), American Society of Nephrology (ASN), UK Kidney Association (UKKA), Canadian Society of Nephrology (CSN), Hong Kong Society of Nephrology (HKSN), Saudi Society of Nephrology and Transplantation (SSN&T), Australian and New Zealand Society of Nephrology (ANZSN), Malaysian Society of Nephrology (MSN),
Track 19: Biopsy
A biopsy is taking one or more samples of the tissue to further examine them under special microscopes to see the samples in greater detail. Kidney Biopsy samples can be taken in two ways one is percutaneous biopsy and open biopsy. A kidney biopsy can be performed by specialists who can be a nephrologist, urologists, transplant surgeons, or interventional radiologists. The percutaneous biopsy is where a needle is placed through the skin that lies over the kidney and is guided to the right place in the kidney, usually with the help of ultrasound. Open biopsy is when a surgery is performed where the kidney sample is taken from the kidney and the sample is sent to a pathology lab to check for the signs of disease. Risks involved in the biopsy are small yet they are advised to be discussed with a medical professional.
Related associations and societies: Malaysian Society of Nephrology (MSN), National Kidney Foundation (NKF), California Dialysis Council (CDC), International Society for Hemodialysis (ISHD), American Society of Transplantation (AST), International Society of Nephrology (ISN), American Society of Nephrology (ASN), UK Kidney Association (UKKA), Canadian Society of Nephrology (CSN), Hong Kong Society of Nephrology (HKSN), Saudi Society of Nephrology and Transplantation (SSN&T), Australian and New Zealand Society of Nephrology (ANZSN)
Track 20: Glomerulonephritis
Glomerulonephritis (gloe-mer-u-low-nuh-FRY-tis) is a group of diseases that cause inflammation of the tiny filters in the kidneys (glomeruli). The function of the kidneys is to remove excess fluid, electrolytes and waste from the blood and pass them into your urine. Glomerulonephritis can come on suddenly or gradually turn into chronic. Lupus and diabetes can cause glomerulonephritis or it can occur on its own. Severe or prolonged inflammation associated with glomerulonephritis can damage the kidneys and treatment depends on the type of glomerulonephritis a patient has. Causes of glomerulonephritis can be infections such as post-streptococcal glomerulonephritis, bacterial endocarditis, viral infections; immune diseases such as lupus, goodpasture’s syndrome, IgA nephropathy; vasculitis such as polyarteritis and granulomatosis with polyangiitis.
Related associations and societies: International Society of Nephrology (ISN), American Society of Nephrology (ASN), UK Kidney Association (UKKA), National Kidney Foundation (NKF), California Dialysis Council (CDC), International Society for Hemodialysis (ISHD), American Society of Transplantation (AST), Canadian Society of Nephrology (CSN), Hong Kong Society of Nephrology (HKSN), Saudi Society of Nephrology and Transplantation (SSN&T), Australian and New Zealand Society of Nephrology (ANZSN), Malaysian Society of Nephrology (MSN)
Track 21: Lupus Nephritis
The condition where the body’s immune system attacks our tissues and organs is termed lupus. Lupus affects skin, kidneys, blood cells, brain, heart, and lungs, and specifically, when it affects the kidneys it is termed lupus nephritis. Healthcare professionals treat lupus nephritis by giving the treatment that helps to reduce inflammation in the kidneys, decrease immune system activity and block the immune cells from attacking the kidneys or making antibodies that attack the kidneys. Early diagnosis of lupus nephritis depends on blood tests, urinalysis, X-rays, ultrasound scans of the kidneys, and sometimes a kidney biopsy. On urinalysis, a nephritic picture is found and red blood cell casts, red blood cells, and proteinuria are found. Drugs like steroids and antimalarial drugs are prescribed for lupus nephritis along with diet changes and monoclonal antibodies.
Related associations and societies: International Society of Nephrology (ISN), American Society of Nephrology (ASN), UK Kidney Association (UKKA), Canadian Society of Nephrology (CSN), Hong Kong Society of Nephrology (HKSN), Saudi Society of Nephrology and Transplantation (SSN&T), International Society for Hemodialysis (ISHD), American Society of Transplantation (AST), Australian and New Zealand Society of Nephrology (ANZSN), Malaysian Society of Nephrology (MSN), National Kidney Foundation (NKF), California Dialysis Council (CDC)
Track 22: Diagnosis and treatment of kidneys
Diagnosis or medical diagnosis is determining the condition based on the symptoms of a person. Medical history and physical examination information are typically collected from the person seeking medical care to find out the diagnosis. In kidney diagnosis, blood tests, age, gender, urine test to measure the levels of waste product called creatinine in the blood are tested. The treatments associated with kidney diseases include hemodialysis, peritoneal dialysis, biopsy, kidney transplantation, and conservative management which treat kidney failure without dialysis.
Related associations and societies: Canadian Society of Nephrology (CSN), Hong Kong Society of Nephrology (HKSN), Saudi Society of Nephrology and Transplantation (SSN&T), Australian and New Zealand Society of Nephrology (ANZSN), American Society of Transplantation (AST), International Society of Nephrology (ISN), American Society of Nephrology (ASN), UK Kidney Association (UKKA), Malaysian Society of Nephrology (MSN), National Kidney Foundation (NKF), California Dialysis Council (CDC), International Society for Hemodialysis (ISHD)
Track 23: Pre-eclampsia and kidney disease
Complications associated with pregnancy which is characterized by high blood pressure are called pre-eclampsia (toxemia). In general, there may be no symptoms but high blood pressure and protein loss in urine are key features in pre-eclampsia. Water retention and swelling of legs are common in pregnant women which make it harder to distinguish it as pre-eclampsia from a normal pregnancy. Women having kidney disease even with mild reductions are at risk of toxemia which might lead to acute kidney injury, endothelial damage, and podocyte loss. Chronic kidney disease may put risk to the development of preeclampsia due to comorbid conditions, such as hypertension, but is also connected with impaired glycocalyx integrity and alterations in the complement and renin-angiotensin-aldosterone systems. Pre-eclampsia is diagnosed before delivery but in some cases, it may begin in the period after delivery which is known as postpartum preeclampsia.
Related associations and societies: American Society of Nephrology (ASN), UK Kidney Association (UKKA), Canadian Society of Nephrology (CSN), Hong Kong Society of Nephrology (HKSN), Saudi Society of Nephrology and Transplantation (SSN&T), Australian and New Zealand Society of Nephrology (ANZSN), American Society of Transplantation (AST), Malaysian Society of Nephrology (MSN), National Kidney Foundation (NKF), International Society of Nephrology (ISN), California Dialysis Council (CDC), International Society for Hemodialysis (ISHD)